I infiltrated the tourist circles of Zanzibar to find out what travellers really know about the most deadly parasite on the planet
Travellers these days are pretty savvy; the ease of international travel and the ubiquity of the internet have encouraged more people to explore the world than ever before, and to be well-informed about the locations they are planning to visit. A key milestone in this travel revolution has been in health; specialized travel clinics tend to the lines of expectant voyageurs, awaiting their roster of immunizations and patiently listening to the lists of do’s and don’ts. The vast, fortunate majority come back with no more than war stories about their first case of “Delhi belly”, or peeling skin, a testimony to the tropical sun. They have dutifully followed the advice about drinking water, haven’t touched raw vegetables and didn’t play with stray cats and dogs. They meticulously applied insect-repellant, slept under bednets and took anti-malarial medication. However, there are exceptions. As a researcher in tropical diseases, I am always amazed when I come across one of the minority; the cowboys who consider malaria a badge of honour, a symbol of truly “experiencing” the tropics, who think yellow fever sounds romantic and amoebas are good company. More to the point, they are often woefully ignorant of some of the basic facts and principles guiding good health while travelling, and so rather than proving their fortitude, are usually the ones ending up in hospital.
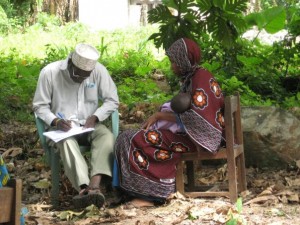
A Ministry of Health worker asks a woman questions during a health survey in Dole, Zanzibar. (Photo © Claire Standley)
Having spent four weeks in the far west of Tanzania studying the distribution of schistosomiasis (one of the so-called neglected tropical diseases, since they tend to take the back-burner in the parade of tropical disease priorities; more on that in the next blog!), I decided to take some R&R in Zanzibar, and first met up with some friends in the backpacker haven of Nungwi, on the northern tip of Unguja island. My friends were all journeying overland through Africa, and, like the conscientious travellers described above, were sensibly concerned about getting sick and ruining their trip, so were taking every possible precaution. Their combined first aid kits would probably have kept an African hospital stocked for weeks! However, as befits the rule, there was an exception. Lovely chap, had travelled extensively over the world, and confidently told me that he wasn’t bothering to take any anti-malarials this trip. When I asked him, disappointed (although not altogether surprised), why this was, he replied that he didn’t need to: after all, he had already got malaria once, and since it was also in Tanzania (just across the strait, in the capital Dar es Salaam), he’s immune to that “strain” and so can’t get re-infected.
Myth number 1 about malaria: Being infected once makes you immune.
BUSTED! You cannot be immune. The species, strain or whatever does not make a difference. Yes, people who have grown up in malaria-endemic areas, and particularly if they were exposed as children, can gain some level of protection, but they can still get the disease. More to the point, if they are removed from the source of infection for a significant period of time (for example they move to a malaria-free zone), they lose that protection, and so become susceptible again.
In any case, I gently told him he was wrong, and probably getting confused with dengue fever (which, incidentally, has the opposite effect; many initial infections are asymptomatic or only result in mild illness. However, a second infection, with a different strain, can leave the patient at greater risk from dengue hemorrhagic fever or dengue shock syndrome, both of which are pretty nasty and can be fatal). They were heading on back to Dar and from there, down to Malawi, so I hoped that he would soon be in the highlands and out of the worst of the malaria transmission area.
I had a few more days of vacation, so made my way down to Paje for a change of scenery. Paje is the kite-surfing capital of Zanzibar, and boasts a stunning stretch of sugar-white sand. While there, unable to stay away from conversations about tropical diseases, I started chatting to a British doctor who was spending the year in one of the two main district hospitals on the island. He informed me of a myth I hadn’t yet heard; apparently, the touts promoting Zanzibar as a paradise destination are prone to telling potential tourists that there isn’t any malaria on the island, in order to encourage them to visit. I had to laugh; there very definitely is malaria on Zanzibar. I had done a bit of work on intestinal worms, in collaboration with the Ministry of Health, and knew that there were on-going diagnosis and treatment programmes as part of the Ministry’s activities. The doctor I was speaking to concurred; he reckoned he saw at least ten cases a week in the district hospital.
Myth number 2 about malaria: There is no malaria on Zanzibar
BUSTED! There most certainly is; while transmission might well be lower than on the mainland, due to a lower population size and fewer mosquitoes, cases do occur and so visitors should remain vigilant about sleeping under bednets, taking preventative medicine and using insect repellant, particularly in the evenings and when going out at night.
In any case, I managed to pass the rest of the night without boring too many other people with details about parasitic infections. The next morning, I sacrificed a few minutes of beach time to check how many dozens of emails had built up over the week I was incommunicado. One of the few interesting ones was from my senior thesis student, Kelly, who is working on a malaria diagnosis study in Mang’ula, several hours south-west of Dar. Her project aims to compare incidences of malaria as determined by two different diagnostic methods: the first, the traditional blood slide, which has to be read under a microscope by a trained technician, and the second, a rapid diagnostic test (RDT) which uses a tiny droplet of blood to test for the presence of antibodies against malaria, indicating an infection. Now, the plenty of trials have been conducted on several of the different formulations of malaria RDT; by and large, all are more sensitive than looking at blood slides, which are known to have low reliability especially when someone has few malaria parasites in their blood. So, usually, the prevalence of malaria infection as detected by RDT is higher than by blood film, though the cases that make the difference are people who have light infections and so not usually feeling that sick anyway. What had surprised Kelly was that in the clinic where she was working, the records showed much higher levels of malaria when people were diagnosed with blood films than with RDTs! In any case, I am hoping she can write her experiences up as a post for malaria.com once all the data is analysed, so you can find the conclusion to the story then.
However, her email had reminded me of a discussion I’d had over breakfast with an ex-pat friend of mine, who is European but has been living in Dar for the last couple of years. Malaria prophylaxis cannot be taken for very long periods at a time – they would get prohibitively expensive, for one, plus the effects of taking the medicine long-term are not well known. So people who live permanently in malarial areas have to rely on other preventative measures; the most effective is sleeping under a long-lasting insecticide treated bednet, which can be purchased for only a few dollars (they are given out for free to many communities in Africa…see the press release about NetGuarantee, a programme run by Malaria No More). Proper bednet usage can reduce malaria transmission by an overwhelming percentage, preventing many cases of the disease; this is particularly important for pregnant women and children, who are most at risk from contracting malaria and suffering severe cases. My friend also mooted another possibility; since malaria drugs can be bought pretty easily over the counter in many places in Tanzania, how about just keeping a few doses around the house and taking them if he gets malaria symptoms?
Myth number 3 about malaria: If I get sick in Africa, it’s probably malaria, so I can treat myself without getting diagnosed.
BUSTED! There is so much wrong with this. First of all, not all malaria is alike. There are different forms of the disease, each caused by different species of the parasite. The major types that infect humans can have subtle variations in their clinical presentations, and, more importantly, are sometimes treated with different drugs. While the go-to cure for most kinds of malaria is chloroquine sulphate, several species of malaria, and most notably Plasmodium falciparum, has become resistant to this form of treatment in some areas of the world. Improper administration of medication, for example not finishing the course of pills, taking the wrong dose or using out-of-date drugs, can assist in the emergence of resistance. Similarly, if you take malaria medication when you don’t really need to (for example, like my friend who might just have a cold), it can contribute to the parasites being able to withstand the drugs in future.
Other types of treatment, such as quinine sulphate, doxycycline and atovaquone-proguanil (sold under the brand name Malarone) may be suitable in some instances as a chloroquine replacement; it is worth noting that if you use Malarone as a prophylaxis, then you can’t also use it to treat malaria if you should happen to become infected. Based on World Health Organisations established in 2006, most chloroquine-resistant malaria is now being treated with artemisinin-based combination therapies, or ACTs. But there’s one more catch; even once you’ve been treated for the initial infection, you may need more medication, depending on the type of malaria you have. Some species, namely P. vivax and P. ovale, have forms that reproduce in the liver; these can lay dormant there for many months and even years, before re-emerging into the bloodstream and causing a relapse of symptoms. The liver stages can be effectively killed with a course of a drug called primequine; however, knowing to take it requires accurate diagnosis, another argument for thinking twice before just taking some drugs at the drop of a fever.

This image shows a traditional "dhow," the sailing ships introduced to Zanzibar and the East African coast by Arab traders over a thousand years ago. They are still used today for fishing and transport. (Photo © Claire Standley)
After my week in paradise, it was time to head back into the dusty interior; to Mwanza this time, to continue my research on schistosomiasis. Spending time with the tourists on Zanzibar reminded me how important it is to continue educating people about the dangers of tropical diseases; it also impressed on me how much at the forefront of people’s minds is malaria, when it comes to thinking about traveller’s health in the tropics. It certainly is one of the most deadly infections, if left undiagnosed and untreated, but it’s also not the only parasite that you can come home with or which can cause significant discomfort during a trip. Given some of these other bugs and worms are favourite research subjects of mine, I’ll use the excuse of my on-going fieldwork in the area around Mwanza to talk about the underdogs of tropical medicine next time!
Hello Claire
Very Interesting article, thank you.
I am currentl yworking down in Mtwara Southern Tanzania as a remote site medic supporting a Port construction facility.
I have a large number of expatriates to care for, and Malaria is a huge concern for me.
I typically see about ten patients a week sith malarial symptoms.
After an initial RDT if I am overly suspicious that a negative result is incorrect I send them to a local clinic for blood slide analysis. Because the clinic ALWAYS diagnose Malaria, I have been asked to prepare thick and thin slides and send them to DAR to a clinic we use for confirmation.
My problem is that in the meantime if the local clinic is wrong, they are on Malaria treatment medication for nothing( you cannot hold back the medication whilst waiting for the audit on the original slide to be done)
My Bigger concern however, is that if I suspect Malaria and I cannot get it confirmed by Laboratory testing, I start them off on treatment ( currently artemether/lumefantrin 20/120) as a precaution. I have done some reading and I believe this is effective against mixed infections?What worries me is your statement about becoming resistant (a bit like antibiotic abuse for colds)
So, to summarise
I have low confidence in the RDT kits we hold here.
The local clinic has a 100% positive rate in everyone we send. ( including one guy who went for something totally unconnected)
I worry that given the symptoms that some people present with, if the RDT test is negative they may still have Malaria. so I start them of on a course of Coartem( such is my clinical guidelines instruction) to be on the safe side.
Do you have any advice? Is there a better way of going about this?
Rgds
Colin
Hi Colin,
Thanks so much for your comment – it is always great hearing from people working in the field and facing the challenges of malaria prevention and treatment every day!
Certainly your story sounds like a familiar one – as you read in the article, my student Kelly also found extraordinarily (and suspiciously) high diagnosis of malaria at the local clinics. It’s great that you are double checking diagnosis from Dar, but I can understand your concerns that your patients are nevertheless in the meantime being pumped full of antimalarial drugs, regardless of whether they need them or not. RDTs are certainly a good way around this, but they do vary significantly in terms of specificity as well as sensitivity. Which brand/type are you using? The World Health Organisation has a great fact sheet about commercially available RDTs, which gives figures for detection probability of both Pf and Pv malaria (unfortunately they don’t seem to have compiled the same data for Pm or Po). So, for example, the ICT combo cassette that Kelly was using in Mang’ula has a decent (85%) probability of detecting 200 parasites per microlitre of blood for P. falciparum infections, but a much much lower probability (<10%) for detecting the same concentration of P. vivax. In Uganda, I worked with the SD combo tests, which have 90% accuracy for both parasites. So, it is worth checking the technical specs of the tests you have, as well as through the literature for studies which have used your test in field settings. The sensitivity and specificity measures should give you a good indication of how much to trust your RDT results (provided you are keeping the buffers at the appropriate temperature, using them correctly, and all those other usual caveats!). One thing specifically to bear in mind is that if you have an RDT that only tests for Pf but you have noticeable levels of Pv/other types of malaria in your area, the RDT won't pick it up but a blood film should. Given that more and more evidence is accumulating to show the importance of non-Pf malaria in sub-Saharan (and particularly East) Africa, it might be worth trying to get your hands on some Pf/non-Pf combo tests to see if that might explain some of the disparity between negative RDT results and clinical suggestions of malaria.
Overall, you are completely right that overtreating can lead to an increase in resistance to malaria drugs; also of concern is that many people with general fever/chills/nausea symptoms are getting treated for malaria when in reality they might have another condition, requiring separate treatment. In particular, I am worried about the outbreaks of dengue which have been on the rise in Tanzania, and that particularly first time infections (i.e. in expats) will be mistaken for malaria. It will be very hard to change the clinics' attitudes toward diagnosis, but something does have to be done. On a short-term scale, one option for you might be to remove the incentive for the clinics to diagnose your workers with malaria, for example by telling them you will be purchasing the drugs elsewhere, and not through the clinic or its local pharmacy. Longer term, the government is going to have to make efforts to ensure its clinic personnel are properly trained in microscopy and aware of the importance of accurately diagnosing malaria. Introducing RDTs alongside blood films has started in some places, which may go some way towards addressing the diagnostic balance.
- C
P.S. Here is the link to the WHO website that details the RDT specifications: http://www.finddiagnostics.org/programs/malaria/find_activities/product_testing/malaria-rdt-product-testing/index.jsp?resubmit=Y&format=table&sel=&pageWidth=1255&NPF=%25&DR=50&DRPV=0&FPR=100&ITR=100&fmt=